RUSP Annual Report 2019–2020
The RUSP Program enrolled 40 new students in the program for the 2019-2020 program year bringing the total currently enrolled to 117 students (66 in Athens, 2 in Cleveland, and 23 in Dublin). We had 15 Clinical Jazz groups (5 in Athens, 1 at Adenain Chillicothe, 1 group at Firelandsin Sandusky, 4 groups in Dublin, 3 in Cleveland and one online group. We have recruited 3 new physician coaches for a total of 20 volunteer RUSP coaches. In 2019-2020, RUSP students represented 12.4 percent of the student body at HCOM.
| Academic Year | 2013–14 | 2014–15 | 2015–16 | 2016–17 | 2017–18 | 2018–19 | 2019–20 |
|---|---|---|---|---|---|---|---|
| Number of students enrolled in RUSP | 20 | 40 | 59 | 84 | 85 | 100 | 117 |
| Total HCOM enrollment | 511 | 610 | 716 | 815 | 922 | 983 | 961 |
| Percent in RUSP | 3.9 | 6.6 | 8.2 | 10.3 | 9.2 | 10.2 | 12.2 |
Professional Development
We offered over 60 hours of professional development on the following topics this year:
- August 12-15 — RUSP Summer Immersion (36 hours)
- Sept 17 — Residency Choice Part 2
- Sept 19 — Visualizing Health Equity
- Sept 26 — Doctor, Can I Trust You? Addressing health Disparities and Implicit Bias in the care of LGBTQ Patients in Rural Communities
- Oct 5 — Specialties of Primary Importance to Rural Communities
- Oct 16 — Telehealth in Urban Underserved and Rural Settings•Oct 23Interrupting the -Isms: Sex, Gender Identity and Sexual Orientation
- Oct 29 — Knowledge is Power: Having research tools in your (doctor) bag of tricks
- Nov 13 — Access to Health Care: Experiences and Perspectives of Deaf Individuals
- Nov 14 — Direct Primary Care in Urban Underserved and Rural Settings
- January 14 — Residency Choices Part 3 –Creating a Rank List•January 16 Interrupting the -Isms: Race and Ethnicity
- January 28 — Zip Code Matters: Health Equity in Rural and Urban Underserved Places
- March 19 — Health Literacy -Relevance in Rural and Urban Underserved Settings
- April 7 — How to help Women Feel Empowered about their Bodies
- April 25 — RUSP Scholarly Endeavors
- May 12 — Residency Choices 1

RUSP Immersion
This year, our Rural and Urban Scholars Pathways program offered a new opportunity for incoming RUSP students, a three-day community-based rural and urban underserved immersion experience. From Aug. 12-15, more than 40 new and returning RUSP students engaged in conversations with RUSP faculty and community members in rural and urban underserved areas in Columbus and in southeast Ohio. We visited the Lower Lights Christian Health Center in Franklinton and learned how Federally Qualified Health Centers work in urban underserved communities. We also heard from community health workers from the Physicians Care Connection. In the afternoon, we learned about accessing community health data and studied health disparities that exist at the county level by looking at adjacent counties with very different health outcomes.
We visited Glouster, Ohio, and had small group discussions with community members. We toured the Tomcat Care Clinic, a school-based health clinic, and discussed the ways this clinic serves the community. We also focused on systems of care in rural and urban underserved communities. We toured Hopewell Hocking Behavioral Health/Primary Care Clinic, a Federally Qualified Health Center; Stagecoach Family Practice, a solo family practice; and Hocking Valley Community Hospital, a critical access hospital.
Scholarly Activity
We had 30 students participating in scholarly activity , mentored by six affiliated faculty during 2019-2020:
Mentored by Sharon Casapulla, EdD, MPH:
- Mangen, J,(OMSIII), Kurtz, C.(OMSI), Amin, R(OMSI), Scriven, E.(OMSI). Athens Community Resource Connections.
- Rambo, C. (OMSIII), Rood, S. (OMSIII), Deagan, K. (OMSIII), Santucci, E (OMSIII), Mapping Health Priorities of Ohio’s Federally Qualified Health Center. Heritage College of Osteopathic Medicine, Ohio University
- Suriel – Peguero, E. (OMSI). What Impact has Osteoarthritis had in Seniors Living in Rural
Communities of Central Appalachia? Heritage College of Osteopathic Medicine, Ohio University - Lussier,L. (OMSI). A Pilot Study for Reminiscence Therapy for Rural Seniors in Appalachian Ohio.
Heritage College of Osteopathic Medicine, Ohio University - Vagedes, R (OMSIII), Webb, E. (OMSIII). HIV Stigma and Knowledge in Rural and Urban Ecuador.
Heritage College of Osteopathic Medicine, Ohio University - Joshi, R., (OMSIII), Jasko, L., (OMSIV), Kolla, S (Resident), Discovering health care needs and role
of primary care for families with children with autism in rural southeast Ohio. Heritage College of
Osteopathic Medicine, Ohio University - Kiger, A., (OMSIII). Gaston, S. (OMSIII). Building an Effective Nutritional Handout for Underserved
Appalachian Ohio. Heritage College of Osteopathic Medicine, Ohio University - Spencer, K. (OMSII). The Implementation of a Brief Educational Intervention to Increase HIV and
HCV Testing among Injection Drug Users in Athens County - Rodriguez, J (Resident), Nandyal, S (OMSIII). Examining Osteopathic medical students’
perceptions of social support. Heritage College of Osteopathic Medicine, Ohio University - Tatum, A (OMSIII), Juka, T (OMSIV). Going back home: Influences on urban medical students
choice to practice in urban underserved communities. Heritage College of Osteopathic Medicine,
Ohio University
Mentored by Melissa Thomas, PhD
- Amstutz, C, (OMSII). Medical Mistrust in Food Insecure Individuals in Appalachia.
Mentored by Rosellen Roche, PhD
- Manzi, J., (OMSIII). Medical Student Perceptions of Mentor-Mentee Relationships with URM Students on the Aspiring DOctors Precollege Program. Heritage College of Osteopathic Medicine, Ohio University
- Manzi, J., (OMSIII) King-Taylor, T., Evaluating the efficacy and student perceptions of a prematriculation educational program for urban and rural underrepresented minority medical students. Heritage College of Osteopathic Medicine, Ohio University
Mentored by Sarah Rubin, PhD
- Frato, G. (OMSIII) Mothers Always Make a Plan: Understanding how culture and poverty shape mothers’ obligations toward child hunger in chronically food-insecure households in Cape Town, South Africa.
- Chapman M.,(OMSIII). Experience of Healthcare Providers Caring for Refugees in Northeast Ohio
- Hines, J., (OMSIII). Exploring Maternal Resistance Birthed from Chronic Stress in African American Mothers at High Risk for Mortality.
Mentored by Dave Drozek, PhD
- Kramer, A., (OMSI). The prevalence of vitamin D deficiency in impoverished communities in northern Lima, Peru, a pilot study
Mentored by Liz Beverly, PhD
- Jivens, M.,(OMSIII). Osteopathic Medical Students’ Understanding of Race-Based Medicine .
- McCollough, K. (OMSIII). Qualitative Diabetes Distress Study.
Mentored by Shannon Nicks, PhD
- Tulisiak, L., (OMSII) Printy, A. (OMSII) Meeting the psychosocial needs of breast cancer survivors:
Examining access to resources in rural Appalachian Ohio
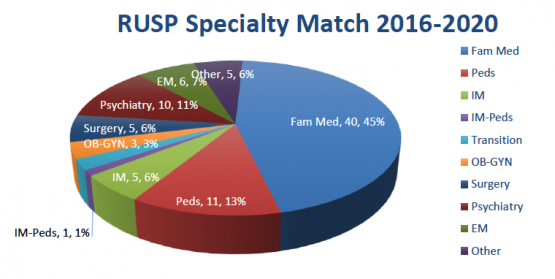
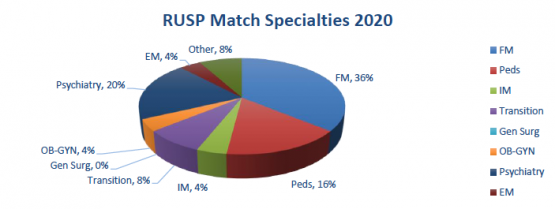
RUSP Match Results
RUSP had 25 graduates in 2020, 56% (n=14) matched in Primary Care (internal med, family med or peds),
36% (n=9) matched in Family Medicine, 64% (n=16) matched in Ohio and 40% (n=10) matched in primary
care in Ohio.
The results of the RUSP End of the year survey has a response rate of 59% (n=70). The results on all items
showed an increase of at least 3 percentage points, suggesting an increase in overall impact and
participant satisfaction. The results of the end of the year survey of all RUSP students highlight the
positive impact the RUSP program has had on the students.
- 76% stated that RUSP increased their interest in primary care
- 51% stated that RUSP increased their interest in practicing rurally
- 80% stated that RUSP increased their interest in practicing in an urban underserved setting
- 80% stated that RUSP increased their interest in residency training in a rural or underserved
- setting
- 95% stated that RUSP enhanced their social development
- 91% stated that RUSP enhanced their academic development
- 96% stated that RUSP enhanced their professional development
- 100% stated that RUSP enhanced their personal development
- 84% stated that RUSP increased their ability to succeed in medical school
- 87% stated that RUSP increased their engagement in medical school
- 91% stated that RUSP increased their satisfaction in medical school
- 91% stated that RUSP increased their knowledge of primary care in rural settings
- 97% stated that RUSP increased their knowledge of health care in medically underserved rural
communities - 86% stated that RUSP increased their knowledge of primary care in urban underserved settings
Student Quotations from the RUSP 2019–2020 End of the Year Survey
- RUSP has been my favorite part about medical school so far. I love that in RUSP, we are able to take a deep dive into the heart of medicine, especially in terms of barriers patients might face when obtaining health care. The most rewarding aspect of RUSP in general is being able to talk with mentors about deeply-rooted health care issues and about what I can do to give the best health care I can in the future. This was facilitated through the Summer program and clinical jazz as well.
- Clinical Jazz sessions were always incredibly grounding and provided a safe space for me to engage with fellow peers and faculty. It was very valuable having insight from peers further along in the medical school journey, and witnessing my own journey throughout the school year. Knowing that I was part of an awesome group of individuals who I had the honor of seeing every month to discuss challenging, yet important topics, was one of the highlights of my first year of medical school and I am very excited to continue this experience for the remainder of my time at OU-HCOM. Truly one of the best and my favorite extracurricular experience in med school!
- Clinical Jazz was really influential in my mental health during Fall semester. We had some very important discussions as a group that helped me to develop my approach to stress and problems early on in medical school. Without these conversations, I think I would have been a lot less happy and potentially have become burned out early on. The summer trip we did to Columbus, Logan, and Glouster really helped me realize the importance and impact of my role in medicine in rural communities and I often reflect on the discussions I had when I'm going through a rough week in medical school to remain focused and motivated.
Cumulatively, the RUSP program has graduated 88 students since its inception (2013, with first graduates
in 2016) and 69% of our graduates entered residency in Ohio (n=61), 65% have chosen specialties with
primary care potential (FM, Peds/IM-Peds, IM) residencies (n=57), and 48% entered primary care
residencies in Ohio (n=42). 18 (20%) of our graduates matched in what we consider ‘generalist
specialties of primary importance to underserved communities’ (OB-GYN, General Surgery, Psychiatry).